Butt Acne: How to Get Rid of Pimples on Your Butt

Introduction
Butt acne, often mistakenly referred to as such, actually encompasses a range of skin issues that cause pimple-like bumps on the buttocks. Unlike facial acne, which is usually caused by blocked pores and too much oil production, butt acne has different underlying reasons.
Taking care of skin problems like butt acne is important for keeping your skin healthy and comfortable overall. Ignoring these problems can lead to discomfort, infections, and even scars. By learning about what causes these bumps and how to treat them, you can greatly improve the look and feel of your skin.
Common causes of butt acne include:
- Folliculitis: An inflammation of hair follicles often due to bacterial or fungal infections.
- Keratosis Pilaris: Characterized by the buildup of keratin in hair follicles, leading to rough, bumpy skin.
- Carbuncles: Larger collections of pus-filled infections that develop from deep folliculitis.
Treatments range from home remedies and over-the-counter products to preventive measures and professional care. This guide will provide practical solutions for managing butt acne effectively, helping you achieve smoother, clearer skin.
Understanding Butt Acne
What is “Butt Acne”?
The term butt acne can be misleading. Unlike facial acne, which results from clogged pores due to excess oil and dead skin cells, butt acne typically refers to various skin conditions causing pimple-like bumps on the buttocks. These conditions include folliculitis, keratosis pilaris, and carbuncles.
How It Differs from Facial Acne
Facial acne primarily arises from blocked sebaceous glands leading to blackheads, whiteheads, and cystic lesions. In contrast, butt acne often stems from:
- Folliculitis: Inflammation of hair follicles due to bacterial or fungal infections.
- Keratosis Pilaris: Buildup of keratin in hair follicles causing rough bumps.
- Carbuncles: Collections of pus-filled infections originating from deeper folliculitis.
Common Misconceptions
Several misconceptions surround butt acne:
- It’s the Same as Facial Acne: As highlighted, the causes differ significantly.
- Poor Hygiene: While maintaining hygiene is crucial, factors like friction from tight clothing and sweating play a more prominent role.
- Only Affects Adolescents: Contrary to belief, individuals across various age groups can experience this issue.
Understanding these distinctions helps in selecting effective treatments and preventive measures tailored for butt acne.
Common Causes of Butt Acne
Folliculitis
Folliculitis refers to the inflammation of hair follicles, often due to bacterial or fungal infections. This condition is a frequent cause of butt acne and can be identified by:
- Symptoms: Small red or white-headed pimples around hair follicles.
- Appearance: These bumps may contain pus, causing discomfort and itchiness.
- Causes: Friction from tight clothing, excessive sweating, and shaving are common triggers.
The inflammation can escalate if not treated properly, leading to more severe conditions like carbuncles.
Keratosis Pilaris
Keratosis pilaris, commonly known as “chicken skin,” occurs when keratin—a protein that protects the skin—builds up in hair follicles. This buildup results in rough bumps on the skin’s surface, particularly noticeable on the buttocks. Key points include:
- Triggers for Flare-Ups: Dry skin, cold weather, and genetic predisposition often exacerbate this condition.
- Manifestation on Buttocks: The rough bumps are usually flesh-colored and painless but can become itchy or inflamed.
Regular exfoliation and moisturizing can help manage keratosis pilaris and reduce its appearance.
Carbuncles
Carbuncles are clusters of pus-filled infections that develop from deeper folliculitis. They are more severe than typical folliculitis and require immediate attention. Characteristics include:
- Development: Arising from untreated folliculitis, carbuncles form when multiple hair follicles become infected.
- Appearance: Larger than regular pimples or boils, carbuncles are swollen, red, and filled with pus.
- Differences from Other Bumps: Unlike other types of acne or bumps, carbuncles are painful to touch and may cause systemic symptoms like fever.
Proper hygiene and avoiding friction can prevent folliculitis from progressing into carbuncles. If you notice persistent or worsening symptoms, seeking medical advice is crucial.
Understanding these common causes is essential for effectively addressing how to get rid of bumps on your booty. Identifying whether you have folliculitis, keratosis pilaris, or carbuncles will guide you towards appropriate treatment strategies.
Identifying Butt Acne Symptoms
Recognizing the symptoms of butt acne is crucial for effective treatment. Visual signs to look for include:
- Redness: This is often the first sign, indicating inflammation and irritation.
- Swelling: Bumps may become swollen, signaling an underlying infection or clogged follicle.
- Pustules: Small, pus-filled bumps that resemble pimples on the face.
- Nodules: Larger, painful lumps under the skin that can be red or skin-colored.
It’s essential to differentiate between various types of bumps on the buttocks:
- Folliculitis: Typically appears as small, red or white-headed pimples around hair follicles. It can be itchy and tender.
- Keratosis Pilaris: Characterized by tiny, rough bumps that may feel like sandpaper. These are usually skin-colored or slightly red.
- Carbuncles: Large, pus-filled lumps that form deep in the skin. They often develop from untreated folliculitis and can be quite painful.
When to Seek Medical Advice
In some cases, butt acne requires professional intervention. Consult a dermatologist if you notice:
- Persistent symptoms lasting more than a few weeks
- Severe pain or discomfort
- Large, pus-filled lumps (carbuncles)
- Signs of infection such as increased warmth, swelling, and redness spreading beyond the initial bump
Timely medical advice can prevent complications and promote faster healing.
Treatment Options for Butt Acne
Warm Compresses
Applying warm compresses can significantly help reduce inflammation associated with butt acne. The heat increases blood circulation, promoting faster healing and reducing the size of the bumps.
Method for Application:
- Soak a clean cloth in warm water.
- Wring out the excess water.
- Apply the cloth to the affected area for 10-15 minutes.
- Repeat this process 2-3 times daily until inflammation subsides.
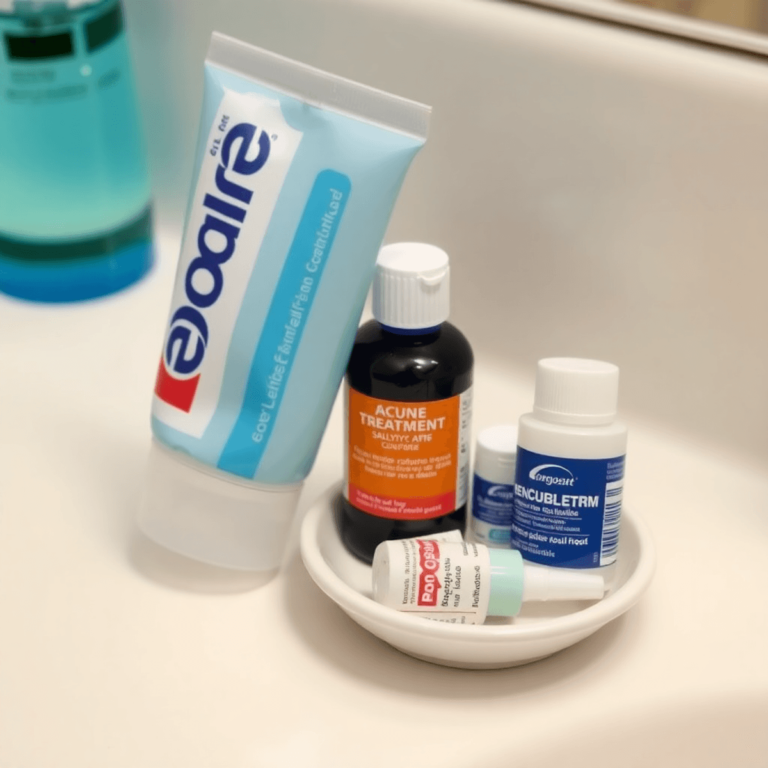
Over-the-Counter Products
Benzoyl Peroxide
Benzoyl Peroxide is highly effective in treating butt acne due to its antibacterial properties. It helps to kill bacteria on the skin surface and reduces inflammation.
Recommended Concentrations and Application Methods:
- Concentration: Opt for products with 2.5% to 5% benzoyl peroxide.
- Application: Apply a thin layer to the affected area once or twice daily. Always start with a lower concentration to assess skin tolerance.
Salicylic Acid
Salicylic Acid works by exfoliating the skin and unclogging pores, making it an ideal treatment for butt acne.
Mechanism of Action:
Salicylic acid penetrates the skin and helps break down dead skin cells and oils that clog pores.
Best Products Containing Salicylic Acid:
- Cleansers: Use a salicylic acid cleanser in the shower.
- Spot Treatments: Apply directly to individual bumps for targeted action.
Natural Treatments
Tea Tree Oil
Tea Tree Oil is renowned for its antibacterial and anti-inflammatory properties, making it an excellent natural treatment for butt acne.
Application Tips:
- Dilute tea tree oil with a carrier oil (e.g., coconut oil) in a 1:10 ratio.
- Apply the mixture to the affected area using a cotton ball.
- Allow it to sit for at least 15 minutes before rinsing off.
- Repeat once daily until improvement is noted.
Zinc Creams
Zinc creams help reduce inflammation and promote healing, effectively treating butt acne.
Role in Reducing Inflammation:
Zinc has natural anti-inflammatory properties that soothe irritated skin and speed up healing processes.
Promoting Healing:
Zinc also aids in cell regeneration, ensuring quicker recovery from acne lesions.
Additional Considerations
While these treatments can be effective, it’s important to remember that some conditions may require more specific care. For instance, if you are dealing with razor burn in addition to butt acne, you might want to explore methods on how to get rid of razor burn.
Moreover, if you’re seeking quick relief from pimples that may also appear on your buttocks, there are proven strategies available for getting rid of pimples overnight.
In certain cases, such as when experiencing severe symptoms or if over-the-counter treatments do not yield results, it’s advisable to consult with a healthcare professional or dermatologist who can provide personalized advice based on your specific situation. For more information regarding common skin issues like acne and their treatments, you can refer to reliable sources such as Medical News Today which offer comprehensive insights into various dermat
Preventive Measures for Butt Acne
Effective preventive measures are essential in maintaining clear and healthy skin on your buttocks. Here, we will delve into practical strategies to reduce the risk of breakouts.
Clothing Choices
Wearing the right clothing can significantly impact the prevention of butt acne.
- Breathable Fabrics: Opt for fabrics like cotton or moisture-wicking materials that allow your skin to breathe. These fabrics help to reduce sweat and moisture build-up, which can lead to bacterial growth and clogged pores.
- Loose-Fitting Clothing: Tight clothing can cause friction and trap sweat against the skin, leading to irritation and breakouts. Choose loose-fitting garments that minimize friction and allow for better air circulation.
Hygiene Practices
Maintaining proper hygiene is crucial in preventing pimples on your butt.
- Showering After Exercise: Sweat and bacteria can accumulate on the skin after physical activity. Showering promptly after workouts helps remove these irritants, reducing the likelihood of breakouts.
- Avoiding Harsh Soaps: Some soaps contain harsh chemicals that can strip your skin of natural oils, causing dryness and irritation. Opt for mild, fragrance-free cleansers that maintain the skin’s natural balance.
- Avoid Fabric Softeners: Fabric softeners can leave residues on your clothing that may irritate sensitive skin areas.
Lifestyle Changes
A few lifestyle adjustments can also play a significant role in preventing butt acne.
- Popping Pimples Risks: It might be tempting to pop pimples, but doing so can lead to scarring and further infection. Allow pimples to heal naturally or seek appropriate treatment methods discussed earlier.
These preventive measures are easy to incorporate into your daily routine and can make a noticeable difference in managing butt acne effectively.
When to See a Dermatologist for Butt Acne Treatment?
Persistent butt acne can be frustrating and sometimes requires professional help. Knowing when to seek medical advice is crucial in effectively managing the condition.
Signs That Indicate the Need for Professional Help
Certain symptoms suggest that it’s time to consult a dermatologist for butt acne treatment:
- Persistent Symptoms: If over-the-counter treatments and home remedies do not improve your condition within a few weeks, it may indicate a more severe or resistant form of acne.
- Severe Pain or Discomfort: Intense pain, especially if accompanied by swelling and redness, could be a sign of an underlying infection that needs medical attention.
- Larger Bumps or Nodules: The presence of large, pus-filled bumps (carbuncles) that do not heal on their own often require professional treatment. You may also experience facial skin bumps which might need specialized care.
- Scarring: If you notice any scarring or skin discoloration due to persistent acne, a dermatologist can provide treatments to minimize these effects.
Overview of Potential Prescription Treatments
Dermatologists have access to a variety of prescription treatments that can effectively address stubborn butt acne:
- Antibiotics: Oral or topical antibiotics may be prescribed to combat bacterial infections causing folliculitis. These medications help reduce inflammation and eliminate bacteria.
Example: Clindamycin or erythromycin are commonly used topical antibiotics.
- Topical Retinoids: These vitamin A derivatives help unclog pores and promote cell turnover, effectively treating and preventing acne. They are particularly useful for treating keratosis pilaris and reducing the appearance of bumps.
Example: Tretinoin or adapalene are frequently prescribed topical retinoids.
- Steroid Creams: For cases involving significant inflammation, mild steroid creams might be recommended to reduce swelling and discomfort.
Example: Hydrocortisone cream can alleviate severe itching and redness.
It’s also important to note that certain butt rashes could mimic acne, but require different treatment approaches. Similarly, if you notice bumps on your arms, it could be related to conditions like keratosis pilaris which also requires tailored treatment.
Consulting a dermatologist ensures you receive tailored treatments based on the specific type and severity of your butt acne. This professional guidance can significantly enhance your skin health and overall comfort.
Conclusion
Managing butt acne effectively requires a combination of awareness, proactive care, and the right treatments. By understanding the causes and symptoms, you can take targeted actions to address this common skin concern.
Taking action early can prevent complications. Here’s how you can start:
- Identify the cause: Knowing whether it’s folliculitis, keratosis pilaris, or carbuncles helps in choosing the right treatment.
- Use appropriate treatments: Over-the-counter options like benzoyl peroxide and salicylic acid are effective for many. Natural remedies such as tea tree oil and zinc creams also offer benefits.
- Adopt preventive measures: Wear breathable fabrics, maintain good hygiene by showering post-exercise, and avoid harsh soaps.
Remember, persistent or severe cases warrant professional advice. Consulting a dermatologist can provide access to more intensive treatments like antibiotics or topical retinoids.
Your skin health is an important aspect of your overall well-being. Taking steps to manage butt acne not only improves your physical comfort but also boosts your confidence. Start integrating these practices today and see the difference in your skin’s health.
FAQs (Frequently Asked Questions)
What is butt acne and how does it differ from facial acne?
Butt acne refers to pimples or skin bumps that occur on the buttocks. It differs from facial acne primarily in its causes and the types of bumps that appear. While facial acne is often linked to hormonal changes and oil production, butt acne can result from factors such as folliculitis, keratosis pilaris, or friction from clothing.
What are the common causes of butt acne?
Common causes of butt acne include folliculitis, which is inflammation of hair follicles often due to bacterial or fungal infections; keratosis pilaris, which leads to rough bumps; and carbuncles, which are clusters of pus-filled infections that can develop from folliculitis.
What symptoms should I look for to identify butt acne?
Symptoms of butt acne typically include redness and swelling on the affected area. It’s important to differentiate between various types of bumps, as some may be harmless while others could require medical attention. If symptoms persist or worsen, seeking medical advice is recommended.
What treatment options are available for butt acne?
Treatment options for butt acne include home remedies like warm compresses to reduce inflammation, over-the-counter products containing benzoyl peroxide or salicylic acid, and natural treatments such as tea tree oil and zinc creams. Each treatment has specific application methods and effectiveness depending on the severity of the condition.
How can I prevent butt acne from occurring?
Preventive measures for butt acne include wearing breathable fabrics and loose-fitting clothing to minimize friction, practicing good hygiene by showering after exercise to remove sweat and bacteria, avoiding harsh soaps that can irritate the skin, and being cautious about popping pimples to reduce the risk of scarring or infection.
When should I see a dermatologist for butt acne?
You should consider consulting a dermatologist if you experience persistent symptoms that do not improve with over-the-counter treatments. A professional can provide a thorough evaluation and may recommend prescription treatments such as antibiotics or topical retinoids tailored to your specific condition.